There’s no shortage of speculation about the promise of AI in healthcare, but one fact to bear in mind is that there’s AI and there’s AI and then there’s AI.
In other words, as Jeff Lagasse puts it more succinctly over at HealthcareFinanceNews, “not all AI is created equally,” and remembering that can prove useful when one tries to determine the impact of AI in healthcare thus far, as opposed to the potential impact yet to come.
For example, notes Lagasse, there’s the “simpler end of the AI spectrum,” which amounts in large part to the efficiencies that have been, and will be, realized through operations automations. On that front, he points to a recent report published in JAMA in which the authors reported the total estimated annual cost of waste in healthcare “was $265.6 billion for administrative complexity alone, including billing and coding waste, and physician time spent reporting on quality measures.”
Further up the spectrum are AI’s predictive capabilities, ever more of which are coming to light via studies in one specialty or medical condition after another.
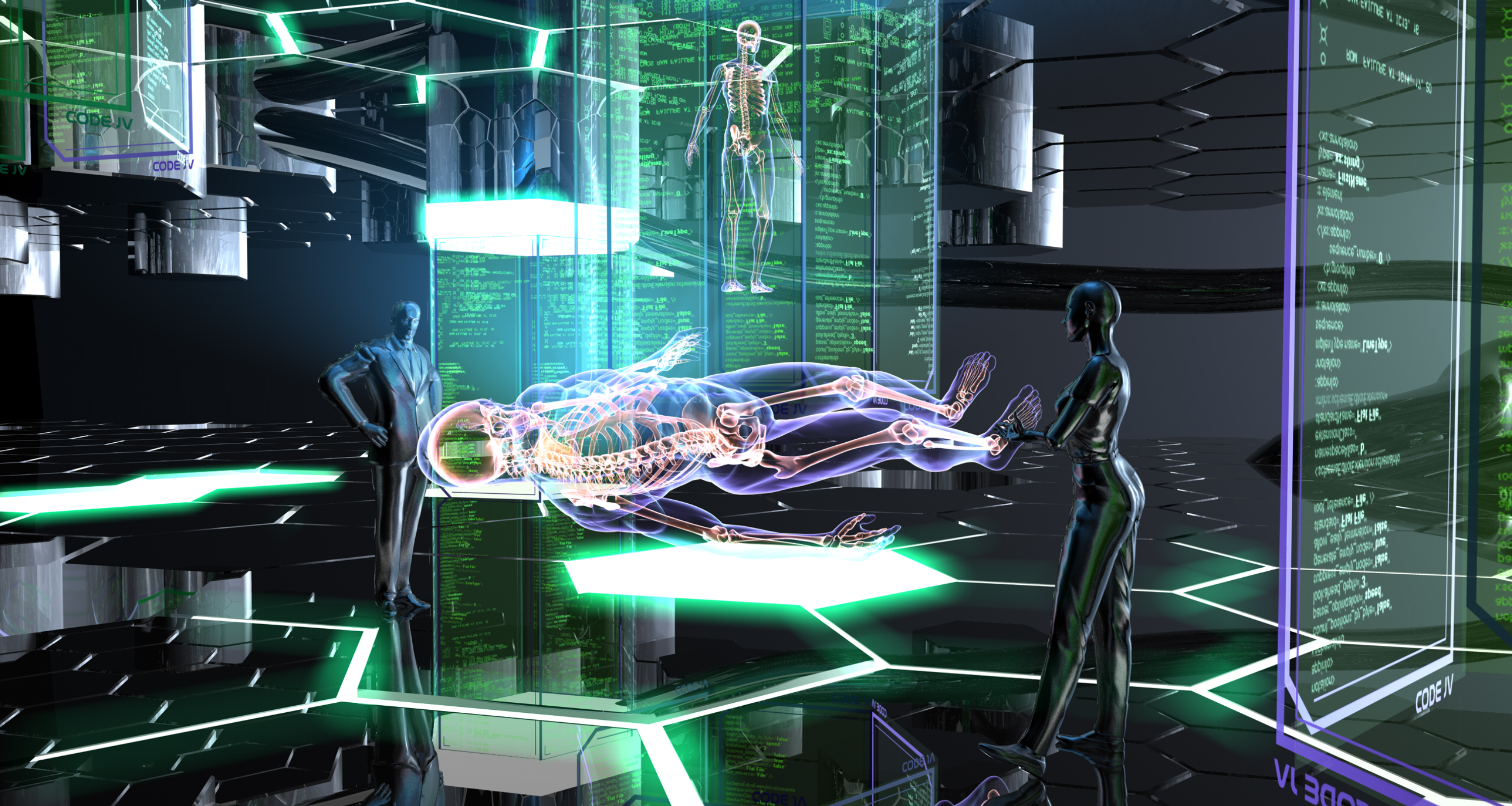
And there’s the highest end of the spectrum: cognitive computing. According ot Venky Ananth, senior vice president and head of healthcare at Infosys, "The value is highest on the cognitive side, but it's also the most difficult to achieve because it needs significant data capability and technical capability to implement.”
One potential role for AI in this capacity, notes Lagasse, is “in the realm of precision medicine by reducing the trial and error associated with matching a patient to a drug. The process can be tricky depending on the specific condition in question.”
For example, diabetes has telltale biomarkers, enabling clinicians to diagnose the disease and propose a specific treatment. But that same predictability isn’t there when it comes to, say, mental disease, for which medicinal prescription can mean an extended period of trial and error.
"What we're working on is, without changing the drug itself, is (finding) a way we can use techniques to pinpoint biomarkers, and through a combination of genomics and metabolism, we match that with a drug, and we figure out the response rate for the drug," said Ananth. "There are some preliminary clinical trials. And then the endgame is, how do we scale this out and roll it out at a larger healthcare industry level?”
That larger level rollout is an ongoing impediment for AI, given the significant expense that often accompanies implementation.
"It doesn't come cheap," Ananth said. The skills to engineer it are huge. It's a tough nut to crack.”
That said, Ananth noted that it’s critical “for healthcare professionals to understand the power of AI and its potential to make them more efficient no matter what role they're in, be it a nurse practitioner, cardiologist or anyone else on the care continuum.”
In short, says Lagasse, AI adoption will be neither simple nor straightforward, but with a sustained and focused effort by healthcare stakeholders, the longterm gains could be massive.


